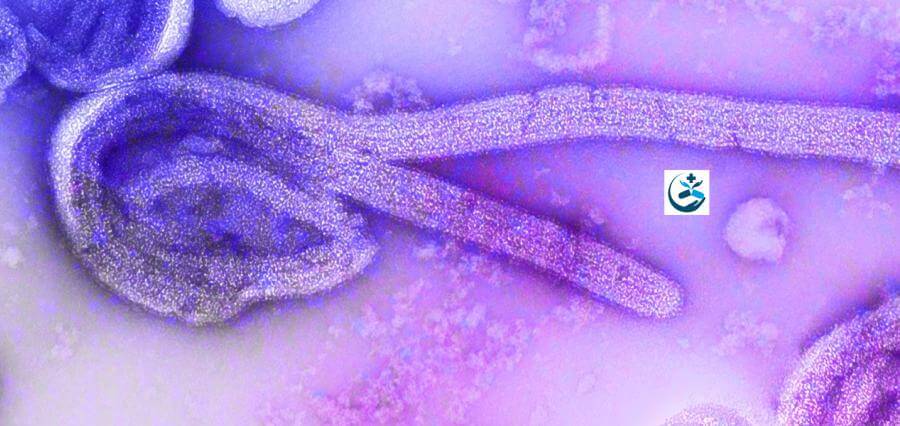
Outbreaks of the Ebola virus disease (EVD) in Zaire have a high mortality and morbidity rate, severely tax the public health systems of the afflicted nations financially and logistically, and have the potential to disrupt global health. The recurrences of EVD in Guinea and the Democratic Republic of the Congo serve as a stark reminder that there is always a chance that it will return.
World Health Organization (WHO) prequalification status has been granted to two vaccine strategies to prevent EVD: the recombinant vesicular stomatitis virus (rVSV)-based vaccine expressing the surface glycoprotein of Zaire ebolavirus (ZEBOV; the rVSVG-ZEBOV-GP vaccine) and the combination of an adenovirus type 26-vectored vaccine encoding the ZEBOV glycoprotein (One dose of the rVSV-G-ZEBOV-GP vaccine has been approved for use in reactive ring vaccination in individuals who are at high risk of exposure during outbreaks; the ring method is used to identify contacts and contacts of contacts.
Recently, a two-dose vaccination regimen called the Ad26. ZEBOV-MVA-BN-Filo combination has been suggested for people who are at some risk for EVD but are not thought to be at high risk. The Partnership for Research on Ebola Vaccinations (PREVAC) consortium in western Africa conducted two randomized, placebo-controlled trials, one involving adults and the other involving children, under a single protocol to evaluate the safety of these vaccines as well as the speed and longevity of antibody responses to these vaccines.
Trials Conducted for Participants
At six locations in four West African nations, eligible adults and children aged 1 to 17 who did not have a history of EVD and who were not pregnant or nursing were enrolled. The protocol includes a complete list of inclusion and exclusion requirements. Adults and adolescents between the ages of 12 and 17 were enrolled first, then kids between the ages of 5 and 11, and finally kids between the ages of 1 and 4.
The Ad26.ZEBOV vaccine (0.5 ml; 510 viral particles), the MVA-BN-Filo vaccine (0.5 ml; 110 infectious units), and the placebo 56 days later were given to participants in the Ad26-MVA group. Other options included the rVSVG-ZEBOV-GP vaccine (1.0 ml; 9.410 plaque-forming units), the rVSVG-ZEBOV-GP vaccine, and the rV Because the vaccinations had different fill volumes, the trial needed two placebos; the placebo groups were combined for analysis.
On days 7, 14, and 28 following the initial dosage of the vaccine or placebo, follow-up visits were conducted. On day 56, the second or booster dosage of the vaccine or a placebo was given. Additional follow-up appointments were followed on days 63 and during months 3, 6, and 12. At each follow-up appointment, the antibody response was evaluated, injection-site responses and symptoms (such as fever and headache) were evaluated through month 6, and information on major adverse events was gathered through month 12.
How does the Antibody respond?
The Filovirus Animal Nonclinical Group (FANG) enzyme-linked immunosorbent test was used to assess serum concentrations of IgG binding antibodies against the Ebola virus surface glycoprotein at baseline and each subsequent visit (ELISA). At month 12, an antibody response—defined as a rise from baseline of at least a factor of four and an antibody concentration of at least 200 ELISA units (EU) per milliliter—was the major immunogenicity endpoint. As in earlier trials, such as the Partnership for Research on Ebola Virus in Liberia (PREVAIL), I trial, the antibody response was defined as an increase from baseline in the antibody concentration by at least a factor of 4.
It was thought that an antibody concentration of at least 200 EU per milliliter and a rise from baseline of at least a factor of 2 would be a correlate of protection. In an examination of immediate response on day 14, we separately evaluated the Ad26.ZEBOV-MVA-BN-Filo and rVSV-G-ZEBOV-GP regimens with placebo.
Read More News: Click Here